Dialectical behavioral therapy (DBT) may improve symptoms of borderline personality disorder (BPD) by teaching skills that include mindfulness and emotion regulation.
Marked by difficulties with emotional regulation, interpersonal relationships, self-image, thoughts of suicide, and other symptoms, living with borderline personality disorder (BPD) isn’t always easy. However, it’s possible to live a happy, fulfilling life with the right kind of treatment and support.
Research shows that the prognosis for BPD is good, especially for those who seek treatment through specialized therapy. The most popular and most effective form of therapy for BPD is dialectical behavioral therapy (DBT). This form of therapy was created for people with borderline personality disorder in mind.
If you’ve been diagnosed with BPD, know that you’re not alone. In fact, it’s estimated that about 1.6% of U.S. adults are affected by this condition.
DBT is a multifaceted treatment approach created by Dr. Marsha Linehan in the early 1990s . Linehan created DBT in hopes of providing relief to those living with BPD, a condition she’s experienced, as she later revealed in her book “Building a Life Worth Living: A Memoir.“
DBT, while created for BPD, has also been helpful for those with:
DBT is a skills-based treatment program broken into four main modules:
Each module consists of various skills that are specific to that module’s theme. Some skills you may learn include:
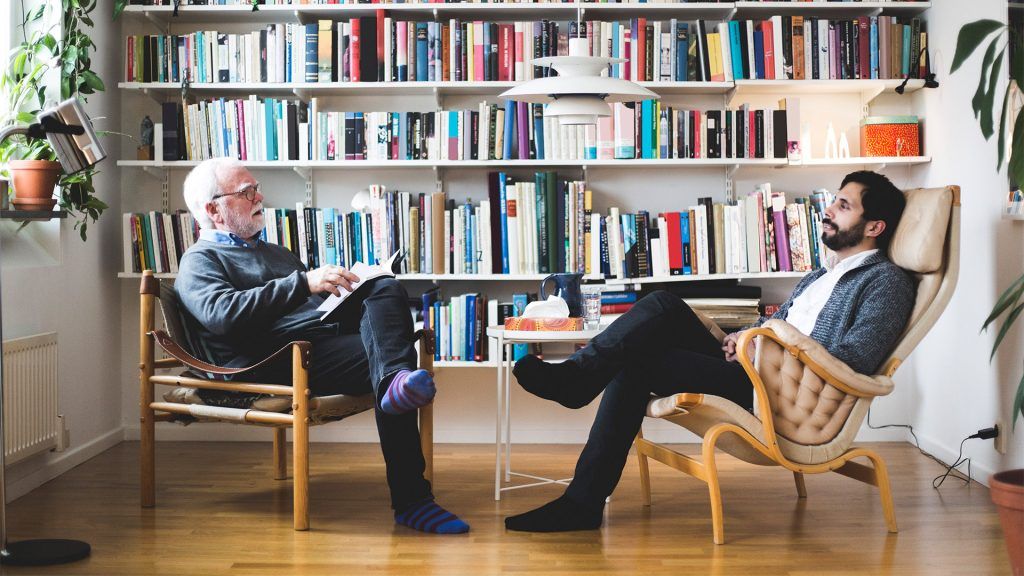
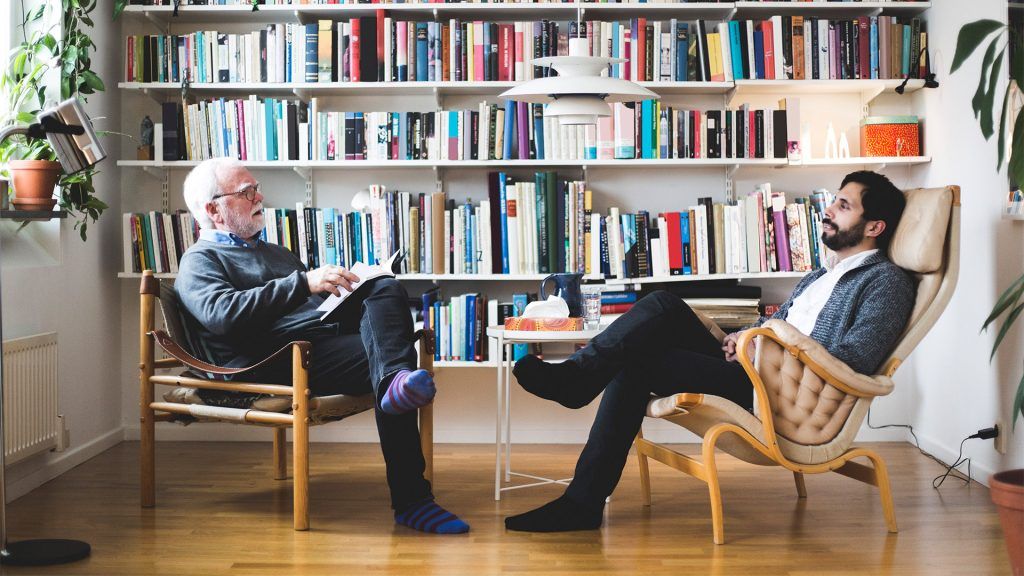
Each module consists of group and individual therapy, as well as homework assignments. Your therapist may also be available for phone coaching in moments where skills may need to be practically applied.
DBT is skills-based, meaning it’s both practical and achievable. Typically, a DBT program lasts 1 year.
Since those with BPD often experience black-and-white thinking, one of the foundations of DBT is literally within its name: dialectics.
Dialectics is defined as holding two seemingly opposite ideas at one time, considering both to be truths. In DBT, “dialectical” refers to the idea of needing both acceptance and change to help improve symptoms. This can bring greater balance and reduce black-and-white patterns of thought.
The other foundation of DBT is mindfulness. Through mindfulness, those living with BPD can learn to make more intentional, conscious decisions and decrease impulsivity and other unhelpful or potentially harmful behaviors over time.
One mindset taught during mindfulness is “wise mind,” which encourages dialectical thinking in crisis and normalcy. It also helps you to attend to your emotions and reason to make wise and balanced decisions.
Ultimately, DBT helps those with BPD both function and flourish in their everyday lives.
Research has shown DBT to be the most effective form of treatment for those with BPD. In fact, one study found that after the first year of treatment, 77% of participants no longer met the diagnostic criteria of BPD.
BPD symptoms such as chronic feelings of emptiness, difficulties with personal relationships, and an intense fear of abandonment tend to be more difficult to treat with DBT — but not impossible.
It’s important to remember that BPD doesn’t look the same for everyone. Different people may have different symptoms, and though DBT may help many people with the condition, it may not work for everyone.